Could research ease night shift’s hazards to heart health?
July 16, 2024
Diana Martinez, Ph.D., an assistant professor in the Department of Biomedical Sciences at Cooper Medical School of Rowan University (CMSRU), has received two grants totaling about $890,000 from the American Heart Association (AHA) and the National Institutes for Health (NIH) to explore the biological link between an increased risk of cardiovascular disease and working night shifts. These projects build on two years of research in her lab at Rowan University.
Our bodies’ 24-hour cycle isn’t just about waking up and going to sleep. Many other physiological factors—metabolism, blood pressure, body temperature—fluctuate in tandem with this daily pattern.
“Working a night shift can cause a misalignment between our activity and our normal biological processes,” Martinez said.
Research has linked the misalignment caused by jobs that take place outside normal working hours with numerous health problems. These conditions include chronic high blood pressure, known formally as hypertension, and itself a risk factor for heart attack and stroke.
Martinez studies a region of the brainstem known as the nucleus of the solitary tract (nTS), which receives information from the body, including the cardiovascular system. One of the functions the nTS monitors, blood pressure, fluctuates naturally over a 24-hour cycle, rising in the morning and reaching its lowest during sleep.
If blood pressure rises too high at any point, neurons alert the nTS by releasing a neurotransmitter called glutamate. When activated by glutamate, the nTS responds by adjusting the heart rate to bring blood pressure back in line. Changes in this feedback system can increase risk of hypertension.
For the AHA grant, a $231,000, three-year award, Martinez plans to conduct experiments with rats examining what happens when changes to the timing of light and dark disrupt the animals’ natural sleep-wake cycle. In this way, they will study how the nTS regulates blood pressure and heart rate, both through the feedback system it governs and independently during the sleep cycle. In addition, they will use this funding to follow up on her previous research suggesting that glutamate levels fluctuate along with the 24-hour cycle in blood pressure.
Likewise, the NIH grant, worth $659,000 over four years, focuses on glutamate communication to the nTS. During misalignment, neuronal signaling into the nTS becomes disrupted, reducing glutamate and thereby making the nTS less able to lower blood pressure. Martinez will investigate one possible contributor to this change: brain cells known as astrocytes, which remove excess glutamate that could otherwise damage the nTS.
When natural rhythms don’t align with those of the environment, Martinez suspects that glutamate-removing proteins on astrocytes become more plentiful. Consequently, she thinks they remove more of the chemical, leaving less available to activate the nTS and, as a result, contributing to increased blood pressure. As part of this grant, she also wants to know how blocking these proteins on astrocytes affects nTS activity over the course of 24 hours.
Understanding these neurological changes may aid in the development of ways to prevent the detrimental effects of working outside normal hours, according to Martinez. These measures could include exercising at a particular time of day, exposure to bright light, or changes to diet.
“The people providing services in our 24-hour world don't have to have developed a slew of health disorders,” Martinez said.
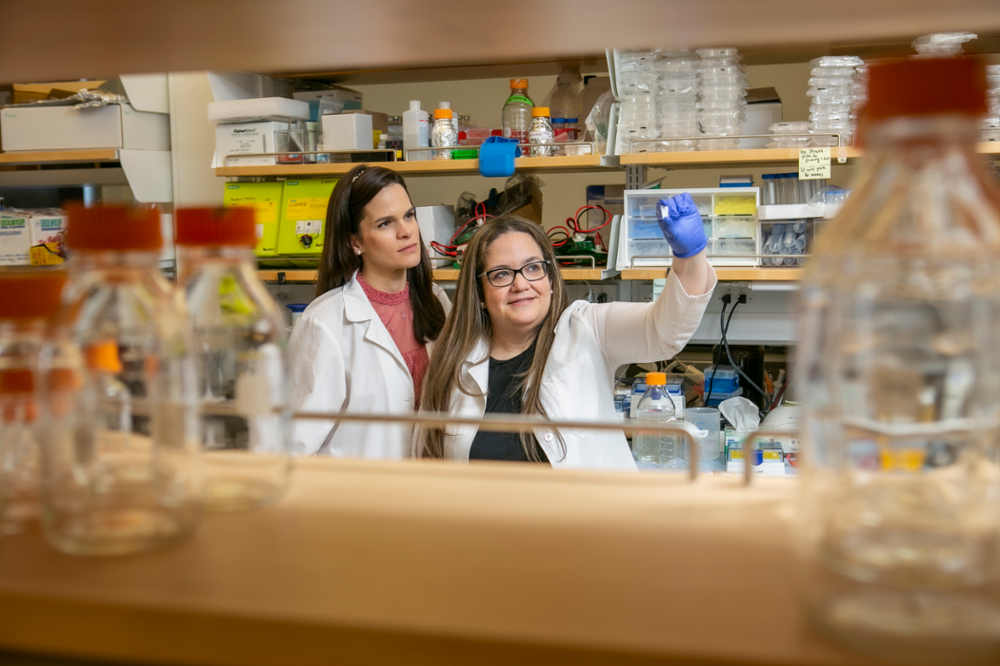
Martinez’s lab at CMSRU began laying the groundwork for this research in 2022. Since then, she has worked to establish a diverse team composed of medical students, undergraduates, and a postdoc, all drawn from CMSRU, Rowan University, Rowan-Virtua School of Osteopathic Medicine and, in one case, Ursinus College in Pennsylvania.
“They drive this work,” Martinez said. “I couldn't do it without them. They think outside the box.”